Transforming Health Claims & Patient, Provider, Payer Experience with Digital Health Claims Platform
The healthcare claims process is ripe for transformation. The traditional paper-based system is inefficient, error-prone, and frustrating for patients, providers, and payers
Are you struggling in high fraud in claims? Does your claims processing takes 4 Hrs to 72 Hrs? Are you spending a lot per claims? Do you manage hospital network /contracts manually? Do you write ICD/DRG/CPT coding manually? Do you do document digitisation manually?
Here are some of the benefits of using a digital health claims platform:
Increased efficiency: Digital claims platforms can automate many of the manual tasks involved in the claims process, such as data entry and routing. This can free up staff time to focus on other activities, such as patient care.
Improved accuracy: Digital claims platforms can help to reduce errors in the claims process. This is because the data is entered once and then shared electronically with all parties involved in the process.
Enhanced transparency: Digital claims platforms provide a more transparent view of the claims process for all parties involved. This can help to reduce disputes and improve communication.
Better patient experience: Digital claims platforms can make the claims process easier and more convenient for patients. This is because they can submit claims online, track the status of their claims, and view their Explanation of Benefits (EOB) electronically.
In addition to these benefits, digital health claims platforms can also help to improve the overall health of the healthcare system. For example, they can help to reduce administrative costs, improve patient outcomes, and make the healthcare system more responsive to the needs of patients.
Here are some examples of how digital health claims platforms are transforming the patient, provider, and payer experience:
Patients: Digital claims platforms can make it easier for patients to submit claims, track the status of their claims, and view their EOBs. This can help to reduce the stress and confusion associated with the claims process.
Providers: Digital claims platforms can help providers to streamline their billing processes and improve their cash flow. This can free up time and resources so that providers can focus on providing care to patients.
Payers: Digital claims platforms can help payers to reduce administrative costs and improve their fraud detection capabilities. This can help to ensure that payers are paying for the care that is actually provided to patients.
Overall, digital health claims platforms offer a number of benefits for patients, providers, and payers. They can help to improve the efficiency, accuracy, transparency, and convenience of the claims process. They can also help to improve the overall health of the healthcare system.
ALFRED HEALTH: NEW AGE AI BASED HEALTH ECOSYSTEM ([PAYER, PROVIDER & PATIENT)
Automated AI & Blockchain Based ALFRED HEALTH Claims Decision System
30Mins to Discharge
ALFRED HEALTH CLAIMS is a AI & Blockchain based decision system for:
Printed, Handwritten, Scanned Document classification
Document digitization & QC
Claim posting and processing
Validation of benefits, rules & conditions
Patient health timeline and profiling for risk assessment
Automated Medical coding like ICD/PCS/
Bills validations with tariff and historical data
Automated AI Based medical evidence & recommendation for treatment, surgery, consultation
AI Based Risk & Fraud intelligence
Integrated provider network platform & Empanelment
Inbuilt QC Platform
Automated settlement and Payment system
+ Many more Unique Modules
Data Driven & Comprehensive Health Provider Platform [For Hospitals, Labs, TPAs etc.]
ABHA | ABDM | HCX Enabled
ALFRED HEALTH PROVIDER & is a end to end data driven platform for Hospitals, Labs & Clinics for:
ABHA integrated for patient adding and patient data consent management
Managing patients, doctors, labs, pharmacies, services
Digital tariff management system inbuilt for payer contracts management
System for OPD, medical consulting with redeem option for OPD Vouchers
360 information for patient vitals, risk, recommendations and patient health timeline
Claims intimation | Cashless Auth | OPD Cashless and more inbuilt systems
Realtime claims update from payers
Comprehensive visibility for claims amount settlement and reconcile with reports
TPA Desk management platform
Integrated system for HIMS/HMS
+ Many more Unique Modules
PRODX DESIGN - No Code Product Benefit & Rule Config in REAL-TIME
NO-CODE Platform
PRODX DESIGN is a end to end NO-CODE Platform for designing rules and product benefit:
Uploading product benefit or connect with any existing
Designing new rules or add existing rules
Modify rules and get activated
Add, Edit or Update policy benefits, limits, inclusions and exclusions
Dynamic rules or combination of rules or benefits
Build & design functional rules for auto-adjudication, controlling the treatment document, process, details
Connecting with Claims and Provider system for instant validation
+ Many more Unique Modules
Automated Digital Tariff Management System With e-Sign Process
NO-PHYSICAL ANYMORE. Manage digitally
ALFRED Tariff SaaS Platform is a end to end NO-CODE Platform for managing digital contracts without ever need of any physical document managing. ALFRED Tariff Helps:
Uploading excel or PDF on system as ONE-TIME to have digital tariff
Manage, edit, approve, update on the fly both side at Payer and Provider. No hassle of physical documents ever.
Update terms and conditions for every tariff digitally
Inbuilt process for e-sign | OTP for freeze
Connected system with provider empanelment
Multiple Tariff at multiple locations to manage for a Provider Group
Automated digitization for tariff and mapping to IRDA/PCS/ICD coding
+ Many more Unique Modules
AI Based Risk & Fraud | ALFRED AI FRAUD PLATFORM
>30% reductions
ALFRED HEALTH FRAUD System is a end to end AI Driven Intelligent Platform that :
Provides comprehensive risk validations and scoring for documents, matching, ICD, PED and more.
Provides historical data driven frauds like price, ICD, Provider, Location, Data Duplication, Document Duplication, Claim Duplication, PED etc.
System analyses medical imaging and cross checks for validations, provides suggested treatment, surgery with recommended cost to avoid high claims cost abuse
Build health risk timeline to validate the historical health trend with current to provide risk & fraud insights.
Document forgery, face & signature related risk & frauds
+ Many more Unique Modules
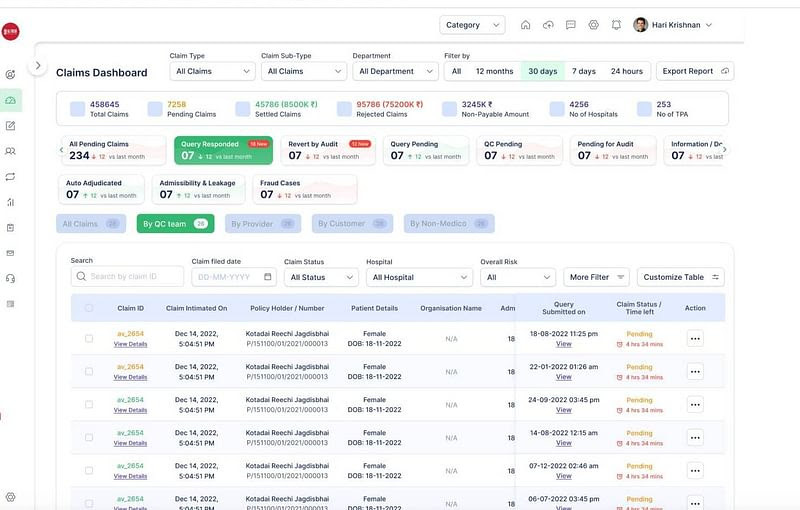
Role Management & QC | Audit Platform for Managing Multiple Stakeholders
Manage anything from internal team like medico, qc, sales, payment etc. to external teams like provider, tpa, labs etc.
ALFRED USER MANAGEMENT is an end to end NO-CODE Platform for managing users, departments and companies for 360 access, communication and operations. This platform helps in:
Controlling access, users, departments, teams
Controlling providers, TPAs, Patient, Investigators
No-Code platform to add, delete, edit or update any user, team, department or company [medico, non-medico, payment, qc, sales, customer service etc.]
Measure team wise, location wise, branch wise performance
Provide approval, rejection and authorisation
QC System to control data entry, accuracy and corrections in real-time
Comprehensive AUDIT system for claims cases, QC, & payments
+ Many more Unique Modules
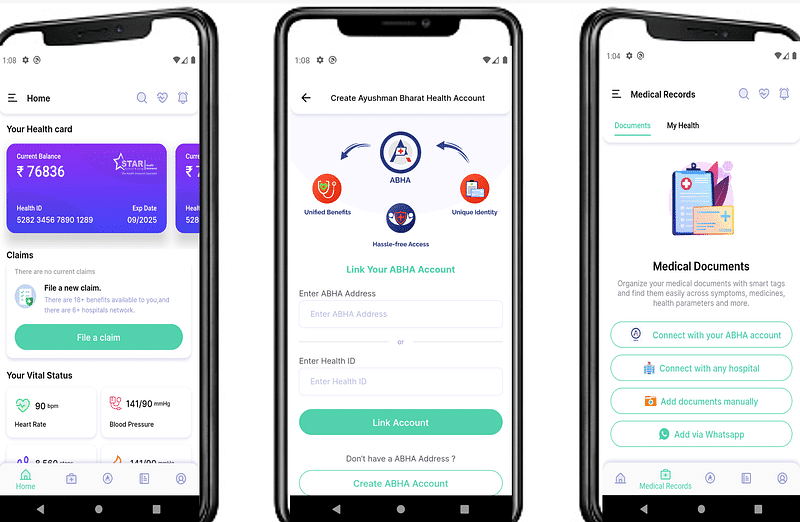
Patient Health 360 App - Designed for Individual or Families
Complete Patient Health App 360 - Manage health, health records and share with consent.
HEALTH 360 is an patient centric app for individual or families that:
Uploading product benefit or connect with any existing
Designing new rules or add existing rules
Modify rules and get activated
Add, Edit or Update policy benefits, limits, inclusions and exclusions
Dynamic rules or combination of rules or benefits
Build & design functional rules for auto-adjudication, controlling the treatment document, process, details
Connecting with Claims and Provider system for instant validation
+ Many more Unique Modules
Here are some of the challenges that need to be addressed in order to fully realize the potential of digital health claims platforms:
Interoperability: The healthcare industry is fragmented, and there is no single standard for exchanging health data. This can make it difficult for digital health claims platforms to communicate with each other.
Security: The security of patient data is a major concern. Digital health claims platforms need to be implemented in a way that protects patient privacy and security.
Cost: The cost of implementing and maintaining digital health claims platforms can be a barrier for some organizations.
Despite these challenges, the potential benefits of digital health claims platforms are significant. As the healthcare industry continues to evolve, digital health claims platforms are likely to play an increasingly important role in improving the efficiency, accuracy, and transparency of the claims process.
ALFRED HEALTH - Enabling Claims Operations Efficient, Automated and Real-Time
GO LIVE IN 60 DAYS
ALFRED is built on great integrations: ALFRED Health is integrated with various tools and applications that easy the deployment and GO-LIVE to our Clients - 20+ apps integrated [out of the box]
Looking for ALFRED Demo. Write to contact@artivatic.ai or aiclaims@alfred.claims
Artivatic Website: www.artivatic.ai
ALFRED HEALTH CLAIMS WEBSITE: alfred.claims